

Introduction: Why Menopause Rarely Looks the Way You Were Told
Ask ten women what menopause feels like, and you are likely to hear ten different stories.
One woman talks about night sweats that arrived suddenly and disrupted years of reliable sleep. Another mentions joint pain that appeared without warning. Someone else describes anxiety she never had before, or a sense that her body no longer responds the way it once did—to exercise, to stress, to food, to rest. Many women experience several of these changes at once. Others notice only one or two. Some barely notice anything at all.
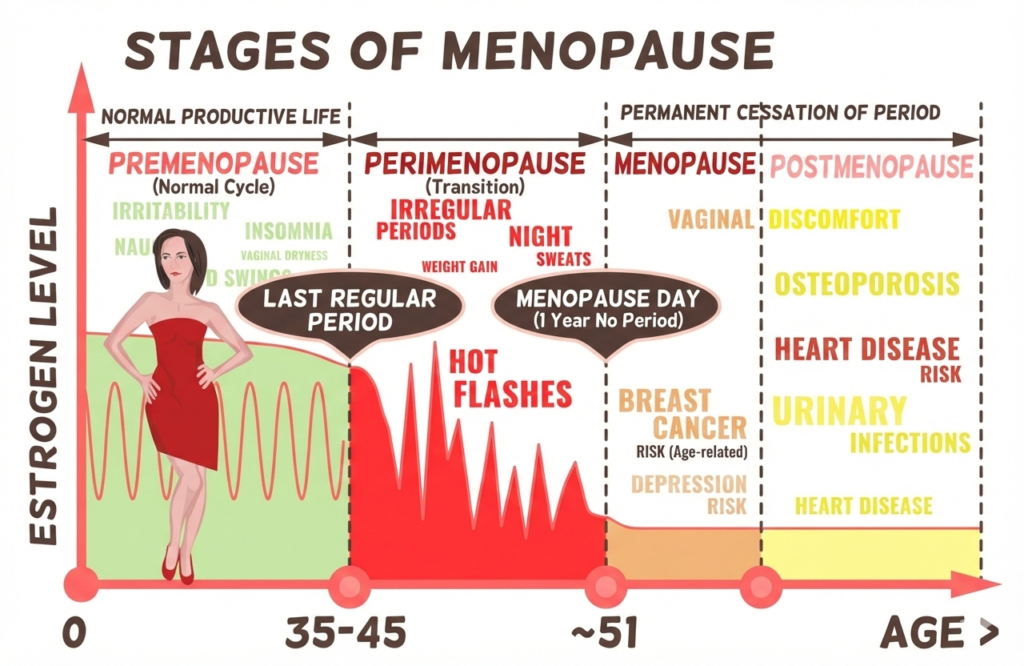
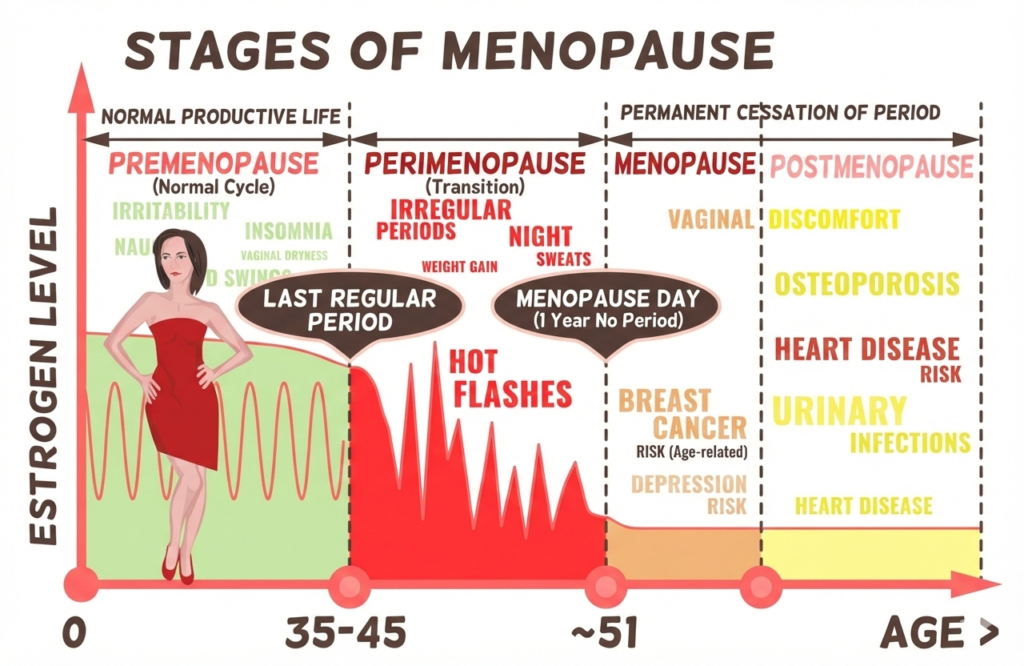
Yet for decades, menopause has been framed narrowly—reduced to hot flashes, missed periods, and an implied sense of inevitability. This framing leaves many women unprepared for the reality: menopause is not a single event, and its symptoms are not confined to the reproductive system.
Menopause is a whole-body transition, shaped by hormones that influence nearly every system involved in energy, mood, movement, metabolism, and cognition. The symptoms that emerge during this transition are not random. They are signals—sometimes subtle, sometimes disruptive—that the body is recalibrating.
Understanding menopause symptoms requires moving beyond checklists and averages. It requires context, biology, and compassion for the fact that no two bodies navigate this transition in exactly the same way.
Core Concept Explanation
What “Menopause Symptoms” Actually Encompass
The phrase menopause symptoms suggests a finite list. In reality, it describes a spectrum of experiences that arise as ovarian hormone production declines and fluctuates, particularly estrogen and progesterone.
These hormones do far more than regulate menstrual cycles. They influence:
- Thermoregulation (how the body manages heat)
- Sleep architecture
- Neurotransmitter balance
- Muscle and connective tissue behavior
- Insulin sensitivity and fat distribution
- Inflammatory signaling
- Stress reactivity
When hormonal signaling becomes less stable, the systems that depend on it respond—sometimes dramatically, sometimes quietly.
This is why menopause symptoms can include:
- Hot flashes and night sweats
- Sleep disruption and early waking
- Mood changes, anxiety, or low mood
- Joint pain and muscle stiffness
- Fatigue and reduced stamina
- Changes in body composition
- Brain fog or reduced concentration
- Heart palpitations
- Digestive changes
Not every woman experiences all of these. Some experience only one. Others notice symptoms that never appear on standard lists.
The common thread is not the symptom itself, but the hormonal context in which it arises.
Why This Becomes Relevant After 40
Biological Factors
For many women, menopause does not begin at menopause.
The transition often starts in the early to mid-forties, during perimenopause, when estrogen and progesterone levels fluctuate unpredictably. These fluctuations—not just low hormone levels—are responsible for many early symptoms.
During this phase:
- Estrogen may spike and crash within short periods
- Progesterone often declines earlier than estrogen
- Feedback loops between the brain and ovaries become less stable
This hormonal volatility affects systems that rely on predictability—sleep, mood regulation, temperature control, and tissue repair.
After menopause, when estrogen levels decline more consistently, symptoms may shift again. Some improve. Others persist. Some appear for the first time.
Lifestyle Factors


Midlife often coincides with sustained external pressure:
- Career responsibility
- Caregiving roles
- Financial stress
- Sleep fragmentation
- Reduced recovery time
These stressors interact with hormonal changes, amplifying symptom perception and physiological load. The body is not simply aging—it is adapting under compounded demands.
Movement & Recovery Factors
Hormonal shifts influence how tissues respond to physical stress. Muscle recovery slows. Connective tissue stiffness may increase. Sleep disruption impairs overnight repair.
Symptoms often worsen not because activity is harmful, but because recovery is insufficient for the current biological state.
What’s Considered Normal
Normal menopause-related symptoms may include:
- Intermittent hot flashes
- Changes in sleep quality
- Fluctuating energy levels
- Mild joint stiffness
- Mood variability
- Changes in weight distribution
Normal does not mean trivial. It means biologically expected, not pathological.
Symptoms often fluctuate, improve, and worsen over time. This variability is a hallmark of the transition, not a failure to cope.
When This May Deserve Attention
Closer attention may be warranted when:
- Symptoms significantly disrupt daily life
- Sleep loss becomes chronic
- Mood changes feel persistent or unfamiliar
- Physical discomfort limits movement or confidence
- Fatigue does not improve with rest
These signals suggest that the body may need additional support—not that something has gone “wrong.”
What Research Suggests Actually Helps
Understanding Before Intervention
One of the most effective interventions is accurate understanding. When symptoms are misinterpreted as decline or personal failure, stress increases—often worsening the symptoms themselves.
Understanding the hormonal basis reframes symptoms as signals rather than threats.
Sleep as a Central Regulator
Sleep disruption both contributes to and results from hormonal shifts. Supporting sleep timing, environment, and consistency often improves multiple symptoms simultaneously.
Movement That Matches the Moment
During menopause, movement supports mood, metabolic health, and joint comfort—but intensity and recovery need recalibration. Consistent, strength-supportive movement often outperforms extremes.
Nutrition as Stabilization, Not Control
Menopause is not the time for aggressive restriction. Stable nourishment supports metabolic signaling and reduces stress reactivity.
Stress Modulation
Chronic stress amplifies hormonal volatility. Practices that reduce sympathetic activation—without adding burden—often have disproportionate benefit.
Common Misconceptions
“Menopause symptoms are all the same.”
They are highly individual.
“If my symptoms are mild, they don’t matter.”
Mild symptoms still reflect systemic change.
“Symptoms mean I’m unhealthy.”
Symptoms often reflect adaptation, not disease.
“Nothing can be done.”
Supportive strategies meaningfully shape experience.
Long-Term Perspective
Menopause symptoms are not a verdict on the future. For many women, symptoms stabilize or improve as the body adapts. Others learn to support their systems more effectively and feel stronger than expected.
The transition is not linear—but it is navigable.
Frequently Asked Questions
Why do menopause symptoms feel so unpredictable?
Because hormonal signaling becomes variable before it becomes low. Fluctuation is more disruptive than consistency.
Can symptoms come and go?
Yes. Many symptoms are episodic and context-dependent.
Why do some women feel symptoms mainly at night?
Hormones interact with circadian rhythms, which regulate temperature, sleep, and stress hormones.
Is it possible to have menopause symptoms with regular periods?
Yes. This is common during perimenopause.
Does exercise always help symptoms?
Often—but only when matched to recovery capacity.
Can menopause symptoms last for years?
For some women, yes. For others, they resolve more quickly.
Final Perspective
Menopause symptoms are not random inconveniences. They are signals from a body undergoing a profound, system-wide recalibration.
Understanding those signals—without fear, without judgment—allows women to respond with clarity rather than frustration. Menopause changes the internal environment, but it does not erase strength, adaptability, or agency.
It simply asks for a different conversation with the body.
Editorial Disclaimer
This article is for educational purposes only. It does not diagnose, treat, or replace medical advice. Menopause experiences vary widely, and readers should consult qualified professionals regarding persistent or concerning symptoms.
